Healthcare Payer Relations: Strategies, Contracting, and Best Practices
The healthcare system operates through two main groups: payers and providers who each serve distinct roles. Understanding these roles helps you navigate the complex healthcare landscape.


Cameron Fletcher
Head of Growth at PayerPrice
Who is involved in healthcare payer relations?
Healthcare payers are organizations that pay for medical services. Payers include Medicare, Medicaid, and private insurance companies that process and pay provider claims. They also include employers and patients who pay directly for care.
Healthcare providers deliver medical services directly to patients. Providers are individuals or organizations that deliver healthcare services to patients. This includes doctors, nurses, hospitals, and clinics.
| Payers | Providers |
|---|---|
| Pay for medical services | Deliver medical care |
| Focus on cost control | Focus on patient treatment |
| Manage financial risk | Manage clinical risk |
| Review claims and coverage | Submit claims for payment |
Payer relations describe the ongoing relationship between health plans and providers. These relationships involve tasks like credentialing, contracting, and payment processing. The success of your healthcare experience depends on how well payers and providers work together.
Strong relationships lead to better patient care and smoother billing processes.
The Current State of Payer-Provider Relationships
58% of healthcare finance leaders report their organization's relationship with payers has become "somewhat negative" or "mostly negative" over the past three years. This statistic reveals the growing tension in payer-provider relationships.
Current relationships remain highly transactional rather than collaborative. You're likely experiencing interactions that focus primarily on annual rate negotiations instead of strategic partnerships.
Payer-provider relations are often strained due to competing financial incentives. Payers aim to control costs while providers seek fair compensation for services. This misalignment creates tension where both sides focus on their own interests rather than collaborating to optimize patient care and outcomes.
Trust Issues
Trust between providers and payers has been fundamentally broken. You may question whether payers act transparently or in your patients' best interests.
Providers lack confidence in payer intent. This creates an adversarial environment where both sides assume negative motives from the other party.
Rising Denial Rates
Some healthcare systems report payer error rates of 30% to 40% in certain denial categories. You're seeing increased challenges with prior authorization and AI-driven denials.
Common frustrating payer practices include:
- Auditing claims years beyond normal timeframes
- Taking back entire claims instead of partial downgrades
- Using algorithms that providers view as flawed
- Systematic approaches to increase denial rates
Data Standardization Problems
Providers face varied reporting requirements across different payers. EHR tools show mixed effectiveness, with only 12.5% of providers finding them "very useful" for patient billing explanations.
Financial Pressures
Inflation rates often outpace reimbursement growth, creating financial strain. Providers are trying to deal with fee schedules that remain largely flat while operational costs continue rising significantly.
The Impact on Patient Care and Experience
When payer-provider relationships break down, patients bear the heaviest burden. Poor communication and trust issues between these parties create real barriers to care that affect your daily healthcare experience.
Delayed authorizations represent one of the most frustrating impacts. You may wait weeks for approval for necessary procedures or medications while providers and payers exchange paperwork. This delay can worsen your condition and increase anxiety.
Billing confusion creates significant stress for patients. When payers and providers don't align on coverage details, you receive unexpected bills or confusing statements. The relationship between health insurance type affects patient experience ratings, showing how payer issues directly impact your satisfaction.
Access to care suffers when relationships are strained. Your provider might avoid certain referrals or treatments due to payment disputes. Some doctors may stop accepting specific insurance plans altogether.
Administrative burdens increase when payer-provider collaboration fails. You spend more time on phone calls resolving coverage questions or resubmitting claims. These issues take time away from actual healthcare.
The payer-provider relationship influences your experience within the healthcare system. The ease of insurance coverage, billing clarity, and care quality all depend on how well these parties work together.
Strong partnerships create smoother experiences. When payers and providers share data effectively, your care becomes more coordinated. Improved payer-provider collaboration benefits patient outcomes by allowing providers to focus on addressing your specific needs rather than administrative tasks.
Contract Negotiation and Management Best Practices
Successful contract negotiations with healthcare payers require extensive preparation and strategic planning. Starting negotiations one year in advance gives you the strongest position possible.
Data-driven negotiations protect your practice's financial health. You must support every contract proposal with concrete evidence and analytics.
Pre-Negotiation Preparation
Collect comprehensive data before entering any payer contract discussion:
- Financial metrics: Current reimbursement rates, payment delays, accounts receivable aging
- Utilization data: Patient volume, service mix, seasonal trends, procedure frequencies
- Cost analysis: Labor costs, overhead expenses, equipment depreciation, supply costs
- Market intelligence: Competitor rates, regional benchmarks, industry standards
- Performance metrics: Quality scores, patient satisfaction ratings, outcome measures
- Claims data: Denial rates, appeal success rates, processing times, down-coding patterns
- Administrative burden: Prior authorization requirements, documentation demands
- Network adequacy: Patient access needs, geographic coverage requirements
- Contract terms: Current fee schedules, annual increases, termination clauses
Understanding Contract Terms
Contract language directly impacts your revenue stream and operational efficiency. Key negotiation elements extend beyond payment rates to include administrative processes and relationship terms.
Watch for problematic contract language including:
- Vague termination clauses that favor the payer
- Broad audit rights without reasonable limitations
- Unilateral rate change provisions
- Excessive hold harmless clauses
- Unclear prior authorization requirements
Price transparency transforms payers negotiations
Automated solutions that integrate clinical and pricing data create unprecedented visibility into healthcare costs and quality metrics.
Key transparency benefits include:
- Clear pricing visibility that eliminates surprise costs and billing disputes
- Data-driven negotiations based on actual market rates and quality outcomes
- Real-time cost comparison tools for better decision-making
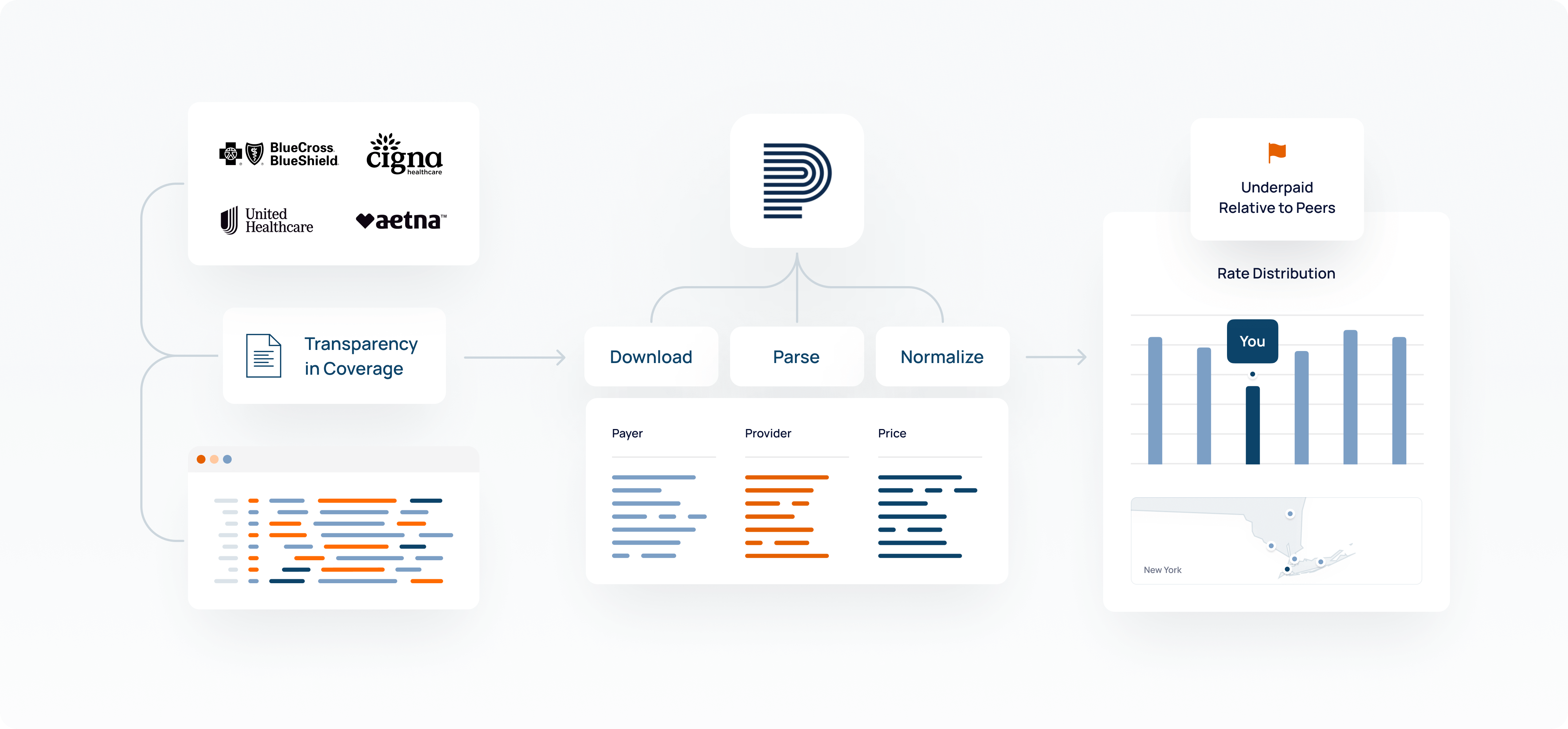
Strategic data use strengthens payer-provider relations through evidence-based pricing strategies. When both parties have access to the same accurate cost information, negotiations become more collaborative and less adversarial. This leads to faster contract agreements and reduced administrative friction.
Price transparency also supports value-based care models and payment integrity. These tools track quality metrics alongside costs, helping close care gaps while ensuring fair compensation. The result is more sustainable payment models that benefit payers, providers, and patients alike.
Are you preparing for your next renegotiation?
Share this article
Help spread the knowledge by sharing with others
Related Articles
Continue exploring healthcare transparency and compliance topics
What is Payer Contract Management? A Complete Guide
Effective payer contract management can result in revenue increases of 1 to 3 percent for healthcare providers.
Payer Contracting: Definition, Best Practices, and Strategic Management
When organizations get strategic about payer contract management, they see real improvements including 4-8% increase in net collection rates and 15-30% reduction in claim denial rates.
Payer Strategy: Best Practices and Insights for Healthcare Success
Organizations with strong payer strategy and contracting approaches see measurable improvements including fewer claim denials, faster payment cycles, and better overall financial performance.
